Four In Five New Zealanders Plan To Get Vaccinated, But Many People Want More Information About Vaccine Safety


Associate health
minister Ayesha Verrall receives the Pfizer vaccine.
Lynn
Grieveson - Newsroom/Newsroom via Getty
Images
Jagadish Thaker, Massey University
New Zealanders’ intention to get a COVID-19 vaccine is at its highest since last year, at 81% of the adult population, according to our latest research.
Ministry of Health surveys, which have been tracking public acceptance of COVID-19 vaccines since last year, also confirm the potential uptake has increased to 80% in May, up from 77% in April and 69% in March this year.
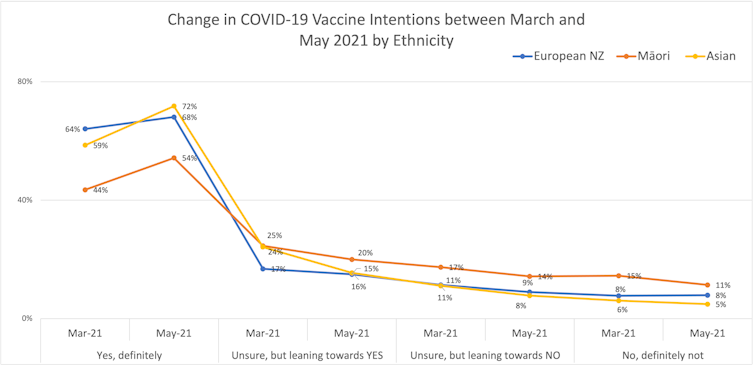
Our longitudinal survey, conducted between March and May, shows an increase by six percentage points among those who will “definitely” take the vaccine to protect themselves and their communities, to 67% in May compared to 61% in March.
The increase is visible across gender, age, education and ethnicity. Among Māori, we see a 10% increase among those “definitely” willing to be vaccinated, from 44% in March to 54% in May.
However, the number of people who say “definitely not” to vaccination remains relatively steady, dropping only slightly to 8% in May, from 9% in March.
The uptick in vaccination intentions is good news, but recent modelling suggests we will need to reach much higher vaccination rates to protect the population from the more transmissible Delta strain.
Author
provided
Of the survey respondents, fewer than a third (27%) have often or very often heard or read the government’s COVID-19 vaccination communication campaign on the radio, in newspapers or on social media in the last month. About four in ten people (43%) have often or very often heard about the campaign on television.
This lack of exposure is worrying. When we asked people who are hesitant or sceptical about vaccination what information they would need to change their mind, 30% said they’d want more information from the government. This is a substantial increase from 18% in March and suggests a low campaign reach.
The most frequently cited information request was for more vaccine safety data. This remained at 30% between March and May. In contrast, there was a sharp decline in the need to see other people take the vaccine first, from 21% in March to 8% in May.
Drop in COVID-19 safety behaviours
We also surveyed participants about the measures they take to protect themselves. The largest decline we observed was in mask wearing, from 64% in March who always, often or sometimes wore a mask in public to 50% in May.
More than three in four respondents continue to use the contact tracing app, down slightly from 78% in March to 76% in May, but encouraging others to use the app has declined from 73% to 66%.
The World Health Organization advises even fully vaccinated people should continue to follow COVID-19 safety behaviours, such as wearing masks in public places.
Misinformation continues to influence people’s decisions, but campaigns to correct it appear to have an impact.
Of the people who watched a misinformation correction video, featuring Auckland GP and advocate for Māori health Rawiri Jansen, 66% said they would definitely take the vaccine, compared to 62% who watched a misinformation video popular among vaccine sceptics on social media channels. The order of watching misinformation and correction does not seem to matter.
The effect of watching a misinformation correction video (just once) appears small, but it highlights the need for continued communication campaigns to address misinformation about the safety, efficacy and regulatory approval of COVID-19 vaccines.
Challenges for the vaccination programme
In several countries, vaccination rates have stalled after an initial uptick.
In the UK, vaccination rates have reduced by 50% recently, primarily due to lack of enthusiasm among the young. In the US, vaccination rates fell just short of President Biden’s target of getting at least 70% of the adult population partly vaccinated before Independence Day on July 4.
Worryingly, the vaccination rates are uneven between US states, and nearly all Americans dying of COVID-19 are unvaccinated.
This has led President Biden to launch a “wartime effort” to vaccinate the country, including door-to-door outreach, vaccination clinics at workplaces, and urging employers to offer paid time off.
Some US states have offered scholarships, million-dollar lottery tickets, free beers and even shotguns as incentives to increase the vaccination rate.
New Zealand is likely to face similar hurdles. While it may be easier to motivate some hesitant people by improving vaccine access and providing services such as paid leave, it will be difficult to reach those with high distrust in government and health experts.
Communities that have been
neglected in conversations about health policies may see the
vaccination effort more as a benefit to the government
rather than a concern for their own and their community’s
well-being. Placing vaccination campaigns with trusted
community members will help, as we have seen when more than
a thousand Pacific people turned up to be vaccinated when
the clinic
was organised with help from their community and held at
their church.![]()
Jagadish Thaker, Senior Lecturer, School of Communication, Journalism and Marketing, Massey University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
![]()


 Binoy Kampmark: Concentrated Markets And Iceless Fokkers
Binoy Kampmark: Concentrated Markets And Iceless Fokkers Binoy Kampmark: Catching Pegasus - Mercenary Spyware And The Liability Of The NSO Group
Binoy Kampmark: Catching Pegasus - Mercenary Spyware And The Liability Of The NSO Group Ramzy Baroud: The World Owes Palestine This Much - Please Stop Censoring Palestinian Voices
Ramzy Baroud: The World Owes Palestine This Much - Please Stop Censoring Palestinian Voices Dee Ninis, The Conversation: Why Vanuatu Should Brace For Even More Aftershocks After This Week’s Deadly Quakes: A Seismologist Explains
Dee Ninis, The Conversation: Why Vanuatu Should Brace For Even More Aftershocks After This Week’s Deadly Quakes: A Seismologist Explains Martin LeFevre - Meditations: Meditation Without A Method
Martin LeFevre - Meditations: Meditation Without A Method Ramzy Baroud: Israel To Annex The West Bank – Why Now? And What Are The Likely Scenarios?
Ramzy Baroud: Israel To Annex The West Bank – Why Now? And What Are The Likely Scenarios?