Ministry reminds people of free flu vaccination
Media Release
7 May 2003
Ministry reminds people of free influenza vaccination
The Ministry of Health is reminding people most at risk of catching influenza this winter to take advantage of the free influenza vaccination before the end of June.
The Ministry annually funds free influenza vaccinations for people in high risk groups, those aged 65 years and over, and adults and children with some chronic health conditions. Influenza can cause serious health complications and even death, and the vaccine is available from most GPs until the end of next month.
Last year about 35,000 New Zealanders suffered influenza-like illness with the worst areas hit being Bay of Plenty, South Auckland and South Canterbury.
"New Zealanders should not be complacent about influenza this winter," says Dr Lance Jennings, National Influenza Immunisation Strategy Group (NIISG) spokesperson.
Nationwide hospital admissions directly due to influenza rose from 379 in 2001 to 487 last year.
Last year about 300,000 New Zealanders received free influenza vaccinations. This year's campaign kicked-off in March and so far the response is similar to last year.
"We've had milder seasons lately but we still want rates of illness to drop. With the cold months now upon us it's important people take advantage of free vaccination so they have optimal protection from influenza," says Dr Jennings.
Dr Jennings says all strains of influenza are easily spread from person-to-person, can lead to serious disease and be life threatening.
BACKGROUND
Chronic medical conditions can include heart disease, stroke and related diseases, ongoing respiratory (chest) diseases like bronchitis or asthma (but only if on regular preventative therapy), diabetes, ongoing kidney disease, most cancers and other conditions including rheumatoid arthritis, organ transplants or HIV/AIDS. For people with these conditions catching influenza can lead to severe complications such as pneumonia which in turn can lead to hospitalisation or death.
Dr Jennings says overseas studies suggest influenza vaccination cuts hospitalisations during the influenza season by half and deaths by two thirds among people aged 65 years and over.
"If you're in one of these risk groups, and are fit and healthy, you're still at risk of being hospitalised or suffering severe complications from influenza, such as pneumonia. Being fit and healthy won't protect you against influenza. The best protection is vaccination.
"Because the virus is always changing we need to update vaccines to provide optimal protection, therefore people must get vaccinated each year regardless of whether they've been vaccinated the year before."
Dr Jennings says influenza is a serious disease that rapidly affects the whole body. "It is easily spread from person to person mainly by sneezing and coughing. Influenza is characterised by sudden onset of fever and chills, cough, body aches and pains, fatigue and headaches."
People who are not eligible for the free vaccination can still talk to their doctor about being vaccinated against influenza. Some businesses subsidise or provide free vaccinations to their employees to decrease winter illnesses.
Anyone wanting more information about influenza can contact their doctor or practice nurse or telephone 0800 IMMUNE (0800 466 863).
ENDS
For further information contact: Kim Purdy Media Advisor Government & Sector Relations\Communications Corporate & Information Directorate Ministry of Health DDI: 04 496 2483 Mobile: 025 277 5411 Fax: 04 496 2010
http://www.moh.govt.nz mailto:kim_purdy@moh.govt.nz
Questions and Answers
What is the Ministry of Health and the National Influenza Immunisation Strategy Group (NIISG) doing to encourage eligible people to be vaccinated? The main role for NIISG and the Ministry of Health is to increase public awareness of influenza and its seriousness. NIISG has developed a variety of user-friendly resources for the public, some of which address myths that are still barriers to people taking up this free vaccination. These are available wherever you get vaccinated.
NIISG has also given health providers resources to help them promote vaccination to all at-risk groups, and established links with relevant organisations such as the Asthma Society and the Diabetes Society to ensure they are given information and resources to pass on to their members.
Who decides if I am eligible for a free vaccination (if I am under 65)? Consultation of patient with general practitioner. He or she is the best person to advise you.
Where can eligible people get a free vaccination? You can get a free vaccination from your local General Practitioner even though a practice nurse may be the one to actually give you the injection. The vaccine is injected into the upper arm and the procedure is fairly painless.
The vaccination is free but what about the doctor's visit? If you are in the at-risk group and visit your doctor's practice for a vaccination before the end of June the vaccine and administration of the vaccine is free. Note that if you see your GP at the same time for any other reason the GP may charge for this service.
How much is the vaccinator funded for each vaccination? Vaccination providers will get $17.69 (incl. GST) from the Government for each vaccination. Eleven dollars of that pays for the work and $6.69 pays for the vaccine.
How many free vaccinations were provided last year? About 300,000 people were vaccinated at a cost to the health sector of some $5,262,000 (incl. GST)
Who manufactures the vaccine? It is manufactured by GlaxoSmithKline and distributed by Healthcare Logistics.
What is influenza? Influenza is a highly infectious illness caused by a virus.
What are the symptoms? Influenza usually causes two or three of the following symptoms: · Sudden onset of fever · Aches and pains · Severe fatigue · Headache · Cough · Sore throat · Stuffy or runny nose
How is it spread? Influenza is very infectious. It spreads through the air by coughing, sneezing and on hands, cups, cutlery or on other objects that have been in contact with an infected person's mouth or nose. Adults are infectious for five days after symptoms occur and children for seven days.
How long does it last? Symptoms usually start to clear up after five to seven days.
How do people tell the difference between the early symptoms of influenza and a bad cold? Influenza will leave you ill for up to 10 days usually suffering from a high fever and requiring bed rest. Patients can also suffer from shivering attacks, muscular pains, headaches, a dry cough, possible vomiting and there can be complications like pneumonia.
You can tell when you are suffering a cold as the symptoms are much milder lasting only 2-4 days. High fever is less common and shivering attacks and severe headaches are rare. Muscular pains and vomiting are infrequent and the cough will be less severe. There is no vaccine available.
How safe is the vaccine? Most people have no reaction to the injection. Occasionally the place where the injection was given is red or sore. Some people may fell unwell for a day or two. These are normal responses to the immunisation.
Has the vaccine been available long enough to prove its safety? It has been avalable since the 1950s.
Does the vaccine provide protection by giving you a dose of influenza? No. The immunisation will not give you influenza because the vaccine contains killed virus.
Does it actually work? Yes. For those at high risk, influenza vaccination reduces hospitalisation by 50 percent and mortality by 70 percent. In general the vaccine is 70-90 percent effective in preventing influenza in healthy adults.
Summary of 2002 influenza statistics During the 2002 influenza season, 3159 consultations for influenza-like illness were reported from a national general practitioner surveillance system. It is estimated that influenza-like illness affected nearly 35,000 New Zealanders during 2002, compared with an estimated 48,000 in 2001. Rates of illness were similar throughout the country and the highest in South Auckland, Bay of Plenty and South Canterbury.
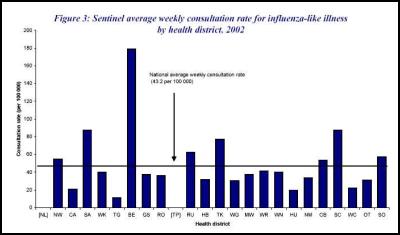
There was an average national weekly consultation rate for 2002 was 43.2 per 100,000 patient population. This rate is the second lowest since rates have been available from the sentinel surveillance period.
How are the statistics collected? There are two parts to the influenza surveillance system in New Zealand - general practice (GP) surveillance and laboratory-based (mainly hospital) surveillance.
General practice surveillance (May to September)
The GP surveillance system started in 1991 as part of the WHO Global Programme for Influenza Surveillance. It is operated nationally by ESR and locally by influenza surveillance co-ordinators in the public health services.
In 2002, national influenza GP surveillance was done from May to September. Local surveillance co-ordinators recruited general practices within their region to participate on a voluntary basis. GPs recorded the number of consultations for influenza-like illness each week and the age group of each of these suspected cases.
Each practice was also asked to collect throat or nose swabs from patients seen with an influenza like illness each week. The swabs were sent to a regional virus diagnostic laboratory and/or ESR for strain identification.
In 2002, 92 GP surveillance practices were recruited from around the country. The average number of practices participating per week was 88, with a total patient roll of 339,954.
Laboratory-based surveillance (year round)
In addition to positive identification of the influenza virus from GP surveillance, year-round surveillance of influenza (and other viruses) is carried out by the four regional virus diagnostic laboratories at Auckland, Waikato, Christchurch and Dunedin Hospitals, and by ESR's virology laboratory. Both the ESR and Auckland Hospital laboratories are designated WHO National Influenza Centres.
Each week, the regional virus diagnostic laboratories report all viral identifications including influenza, largely from hospital in-patients and outpatients, to ESR, where the data is collated and reported nationally.
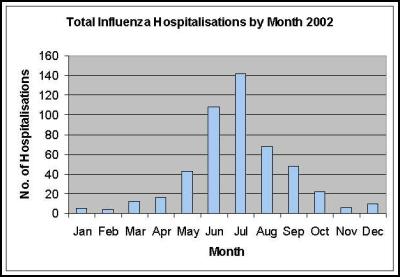
In 2002, there were a total of 483 hospital admissions for influenza. This compares with 379 admissions in 2001. Figure 3 shows these admissions by month, of which occurred during May to September. The highest number of admissions occurred in June and July.
The next graph shows the GP surveillance average weekly consultation rates for each district during May to September 2002. The district reporting the highest rate was Bay of Plenty (178.65 per 100 000 patient population), followed by South Auckland (87.46 per 100 000) and South Canterbury (87.34).
Click For Big
Version
Health Districts: NL Northland, NW North West Auckland, CA Central Auckland, SA South Auckland, WK Waikato, BE Eastern Bay of Plenty, RO Rotorua, TG Tauranga, GS Gisborne, RU Ruapehu, TP Taupo, HB Hawkes Bay, TK Taranaki, MW Manawatu, WG Wanganui, WN Wellington, WR Wairarapa, HU Hutt, NM Nelson-Marlborough, CB Canterbury, SC South Canterbury, WC West Coast, OT Otago, SO Southland.
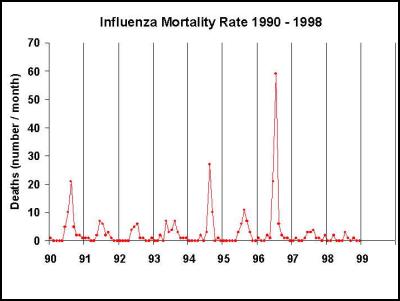
The next graph shows there were 307 influenza fatalities recorded during a nine year period from 1990 to 1998. In 1999, influenza caused 27 deaths. Deaths peaked at 94 during the 1996 influenza epidemic.
There is some difficulty and delay getting good mortality data for influenza. Most people who die following influenza are admitted to hospital because of an exasperation of a chronic condition such as diabetes or heart disease. People often die of complications from these conditions or from pneumonia and the death certificate more often than not cites the chronic disease as the cause of death. Some data is collected from coroner's reports and this can take a long time to come in.
In general mortality directly due to influenza is grossly under reported.
ENDS


 University of Auckland: Screentime Rules Reduce Childhood Obesity Risk
University of Auckland: Screentime Rules Reduce Childhood Obesity Risk OraTaiao: Health Sector United In Opposition To The Treaty Principles Bill
OraTaiao: Health Sector United In Opposition To The Treaty Principles Bill RNZ: New Podcast - Kim Hill Wants To Know
RNZ: New Podcast - Kim Hill Wants To Know Buy NZ Made: Beware The Black Friday 'Deal'
Buy NZ Made: Beware The Black Friday 'Deal' Little Miracles Trust: 60 Landmarks Light Up Purple To Support Babies Fighting For Life On World Prematurity Day
Little Miracles Trust: 60 Landmarks Light Up Purple To Support Babies Fighting For Life On World Prematurity Day Maia Studio: Frankie Venter Performs With Coldplay At Sold Out Eden Park Show
Maia Studio: Frankie Venter Performs With Coldplay At Sold Out Eden Park Show